Free shipping £150+ Orders
What Causes Hyperpigmentation on Face and How to Fix It
Hyperpigmentation is simply the term for patches of skin that become darker than the surrounding areas. It happens when your skin produces too much melanin, the natural pigment that gives skin, hair, and eyes their colour.
This overproduction can be sparked by a whole range of things, from sun exposure and inflammation to hormonal shifts, all leading to those familiar dark spots and uneven patches.
What Exactly Is Hyperpigmentation?

If you’ve ever dealt with stubborn dark spots after a breakout, sun spots that pop up after a holiday, or patches of discolouration, you’ve experienced hyperpigmentation firsthand. It’s an incredibly common condition where certain areas of skin simply become darker than the rest.
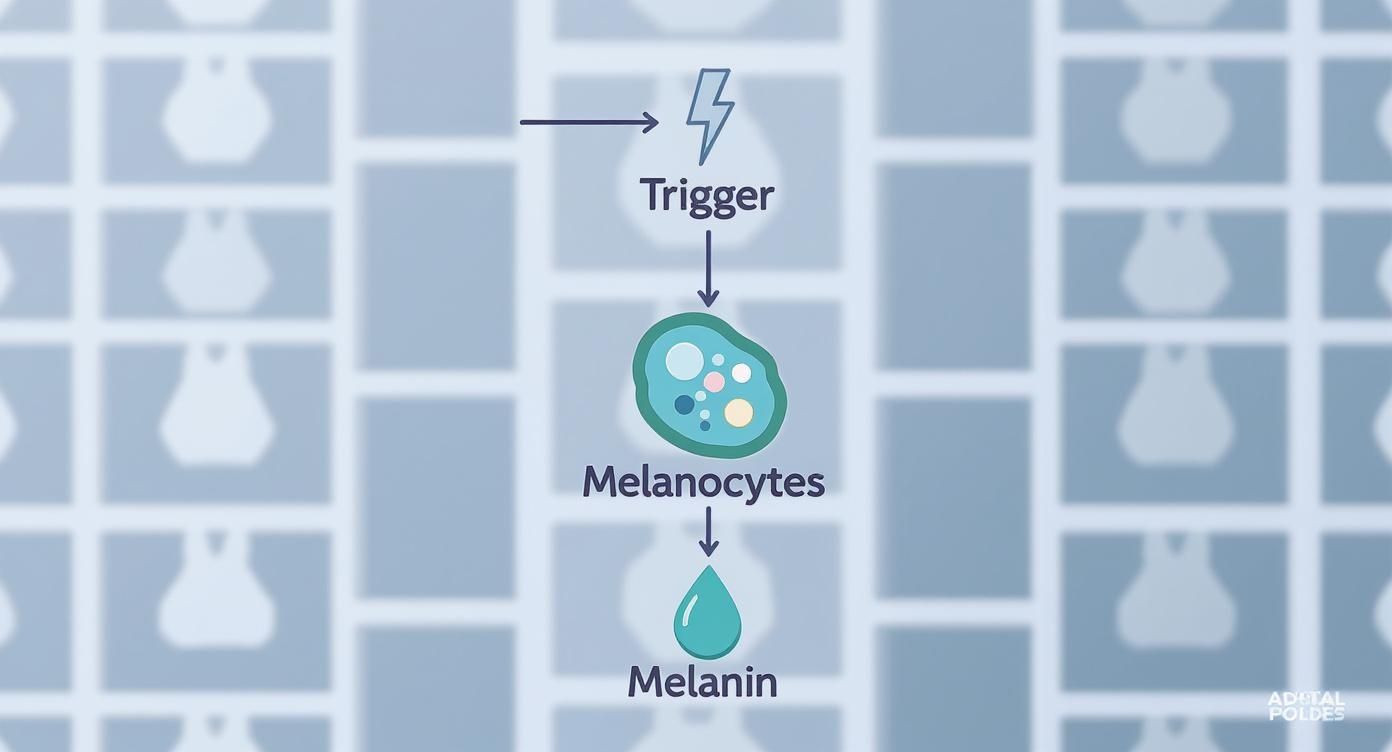
This all comes down to specialised skin cells called melanocytes. Think of them as tiny, highly controlled pigment factories dotted throughout your skin. Their job is to produce melanin and distribute it evenly to give you a uniform complexion. But when certain triggers come into play, these factories can go into overdrive in specific spots.
The Key Triggers Explained
When your skin faces a trigger, these melanocyte cells start producing an excess of melanin. This extra pigment can then clump together, creating visible deposits that show up on your skin’s surface as dark marks.
The main culprits behind this process are:
- Sun Exposure: UV radiation from the sun is the single biggest trigger. Your skin produces melanin to try and protect itself, and too much sun leads to an over-enthusiastic response.
- Inflammation: Any kind of skin trauma—like a spot, a cut, a rash from eczema, or even aggressive scrubbing—can kickstart melanin production, leaving a dark mark long after the initial injury has healed. This is known as post-inflammatory hyperpigmentation (PIH).
- Hormonal Changes: Shifts in hormones, particularly during pregnancy or from taking oral contraceptives, can trigger a specific type of blotchy hyperpigmentation called melasma.
This isn’t a rare issue; it’s practically universal. Facial hyperpigmentation affects over 90% of adults by age 50 worldwide, making it one of the top cosmetic concerns we see in the UK. Here, melasma in particular affects a significant number of women, showing up as brown or grey-brown patches that often get worse in the sun. To get a better sense of how to manage this, you can explore more insights on hyperpigmentation treatments in the UK.
Hyperpigmentation isn’t just a surface-level cosmetic problem; it’s your skin’s way of signalling that it’s been under stress. Getting to grips with what’s causing it is the first, most critical step towards getting a clearer, more even complexion.
To make things a bit clearer, here’s a quick breakdown of how different triggers lead to different types of hyperpigmentation.
Quick Guide to Hyperpigmentation Triggers
| Primary Trigger | Resulting Type of Hyperpigmentation | Common Appearance |
|---|---|---|
| UV Radiation (Sun) | Sun Spots / Solar Lentigines | Small, defined, flat brown or black spots on sun-exposed areas like the face and hands. |
| Inflammation (Acne, Eczema, Injury) | Post-Inflammatory Hyperpigmentation (PIH) | Flat spots of discolouration (pink, red, brown, or black) left behind after a wound or spot has healed. |
| Hormonal Fluctuations | Melasma | Symmetrical, blotchy brown or grey-brown patches, often on the cheeks, forehead, nose, and upper lip. |
| Ageing Process | Age Spots / Liver Spots (Lentigines) | Similar to sun spots, these are small, dark areas that appear on skin that has had years of sun exposure. |
| Genetics / Medical Conditions | Freckles / Underlying Health Issues | Can range from clusters of small spots to more widespread, irregular discolouration linked to specific conditions. |
Understanding these distinctions is key. Once you know what’s causing the hyperpigmentation on your face, you can start to build an effective plan for both preventing new spots and treating the ones you already have.
The Science Behind Your Skin’s Dark Spots
To get to the bottom of what causes hyperpigmentation, we need to look at what’s happening beneath the skin’s surface. It all begins with highly specialised cells called melanocytes – think of them as your skin’s own personal pigment factories.
These cells live in the deepest layer of the epidermis, and their main job is to produce melanin, the natural pigment that gives your skin, hair, and eyes their unique colour.
You can picture melanocytes as tiny, diligent workers. Normally, they produce a consistent amount of melanin, which gets neatly packaged up and sent out to neighbouring skin cells. This ensures your skin tone is even and, crucially, provides a baseline level of protection against the sun’s UV rays.
How Triggers Throw Things Off Balance
Hyperpigmentation occurs when this well-oiled machine gets a disruptive signal. When your skin faces a trigger, like prolonged sun exposure or the inflammation from a particularly angry spot, it essentially sends out an S.O.S.
This distress call puts the melanocytes into overdrive. They start churning out far more melanin than usual in that specific area. All this excess pigment clumps together, creating a dense, concentrated patch of colour.
The dark spot you see on your skin is the visible evidence of this internal chaos. It’s not just a mark on the surface; it’s a sign that the pigment-producing cells in that spot have been over-stimulated by a past event.
This overproduction is the true root of what causes hyperpigmentation on the face. It’s a defence mechanism gone a little too far, leading to an unwanted cosmetic issue.
The Role of Genetics and Skin Tone
Your genes also have a say in how likely you are to develop hyperpigmentation. Some people simply inherit more sensitive melanocytes that react more dramatically to triggers like UV rays or inflammation.
And while anyone can experience hyperpigmentation, it can look and behave differently depending on your natural skin tone.
- Lighter Skin Tones (Fitzpatrick I-III): Tend to be more susceptible to sun spots, also known as solar lentigines, and freckles as a direct result of sun damage.
- Deeper Skin Tones (Fitzpatrick IV-VI): Naturally have more active melanocytes. This makes them more prone to post-inflammatory hyperpigmentation (PIH) after things like acne, a cut, or a rash. These marks often appear darker and can take much longer to fade.
Grasping this basic science is empowering. When you understand that dark spots are a response to specific signals, you can see why certain treatments work. For example, ingredients like mandelic acid help by accelerating cell turnover, encouraging the discoloured surface cells to shed more quickly. To really see results, it’s important to know how to use mandelic acid as part of a consistent routine.
What’s Causing The Dark Spots on My Face?
So, we know that hyperpigmentation is just our skin’s pigment-producing cells, the melanocytes, going into overdrive. But what’s actually flipping that switch? Pinpointing the specific trigger behind your dark spots is the first real step toward getting them under control. Often, the culprit is a daily habit or a change happening inside your body.
No matter the cause, the core process is the same: something signals your melanocytes to pump out too much melanin in one concentrated area.
Let’s break down the most common triggers you’re likely to encounter.
Sun Exposure: The Main Offender
Let’s be clear: unprotected sun exposure is, hands down, the number one cause of hyperpigmentation. When UV rays hit your skin, your melanocytes kick into gear, producing melanin to create a tan, which is your body’s attempt to shield itself from further damage.
Think of it as your skin’s own, slightly imperfect, sunblock. The problem is that after years of this, the system gets overwhelmed. Melanin production becomes patchy and uneven, leading to those distinct dark spots we call solar lentigines—or, more commonly, sun spots and age spots.
You’ll typically see them pop up on the high points of your face where the sun hits first: your cheeks, nose, and forehead. And don’t underestimate incidental exposure from driving or sitting near a window; it all adds up. If you’re already dealing with marks from the sun, our guide on how to treat sun-damaged skin is a great place to start.
Post-Inflammatory Hyperpigmentation (PIH): The Aftermath of Skin Trauma
Ever had a pesky spot finally heal, only to leave a stubborn dark mark in its place for months? That’s Post-Inflammatory Hyperpigmentation, or PIH. It’s your skin’s memory of an injury.
When your skin is traumatised—from acne, eczema, a simple scratch, or even a harsh skincare treatment—it sets off an inflammatory cascade. This process revs up the local melanocytes, which then deposit excess pigment, leaving a flat discoloured patch long after the original problem has gone.
PIH is a major concern here in the UK, particularly for those with deeper skin tones who are naturally more prone to it.
Hormonal Changes: The Story of Melasma
Sometimes, the trigger isn’t external at all. Melasma is a classic example of hormonally-driven hyperpigmentation, which is why it’s often nicknamed the “mask of pregnancy.”
It shows up as symmetrical, blotchy brown or greyish patches, usually on the cheeks, forehead, chin, and above the upper lip. The biggest hormonal triggers are:
- Pregnancy: A surge in oestrogen and progesterone can put melanin production into high gear.
- Hormonal Contraception: The pill and other hormonal methods can have the same effect.
- Hormone Replacement Therapy (HRT): This can also contribute to the development of melasma.
For many people, getting a handle on their hormonal health is key. Understanding your personal profile can shed light on the root cause, and you can even look into options for hormone level testing at home for deeper insights.
A crucial point about melasma: the sun is its amplifier. Even a tiny amount of UV exposure can make existing patches significantly darker. This makes relentless sun protection an absolute non-negotiable for managing it.
Other Factors to Consider
While sun, inflammation, and hormones are the big three, a few other factors can play a role. Certain medications, for instance, can make your skin more sensitive to the sun (a condition called photosensitivity), leading to dark patches.
And of course, there’s genetics. If freckles and sun spots run in your family, you’re likely more susceptible yourself.
Recognising the differences between these types is key to finding the right solution.
Comparing Types of Facial Hyperpigmentation
To help you identify what you might be seeing on your own skin, this table breaks down the key characteristics of the most common forms of facial hyperpigmentation.
| Type of Hyperpigmentation | Primary Cause | Typical Appearance on Face | Most Affected Demographics |
|---|---|---|---|
| Solar Lentigines (Sun Spots) | Chronic UV exposure | Small, defined, light brown to black flat spots on sun-exposed areas like cheeks and nose. | Primarily individuals over 40 with a history of sun exposure, but can appear earlier. |
| Post-Inflammatory Hyperpigmentation (PIH) | Inflammation or injury (e.g., acne, eczema) | Flat, irregular patches of tan, brown, or purplish discolouration where an injury occurred. | More common and persistent in individuals with deeper skin tones (Fitzpatrick types IV-VI). |
| Melasma | Hormonal fluctuations (e.g., pregnancy, birth control) exacerbated by UV exposure | Symmetrical, blotchy, mask-like patches of brown or greyish-brown skin, often on the forehead, cheeks, and upper lip. | Predominantly affects women of reproductive age; often triggered during pregnancy. |
| Freckles (Ephelides) | Genetics and sun exposure | Small, light brown or reddish spots that darken with sun exposure and fade in winter. | Most common in individuals with fair skin, red or blonde hair, and a genetic predisposition. |
By understanding these distinctions, you’re better equipped to identify the potential cause of your dark spots and seek the most effective path forward for treatment and prevention.
Your First Line of Defence Is Prevention
While it’s great to know there are treatments for dark spots, the best strategy is always to stop them from appearing in the first place. You’ve already done the hard part by understanding what triggers hyperpigmentation; now, it’s about putting that knowledge into practice.
Building a protective routine doesn’t mean adding ten complicated steps. It’s all about consistency and creating a few simple habits that become as automatic as brushing your teeth. Committing to these daily practices won’t just keep new spots at bay—it will boost your skin’s overall health and resilience for years to come.
Make Sun Protection Non-Negotiable
If you take only one piece of advice from this guide, let it be this: daily, year-round sun protection is the single most important thing you can do to prevent hyperpigmentation. Full stop. UV radiation is the number one trigger for excess melanin production, making a good sunscreen your best friend.
And I don’t just mean for sunny days at the beach. UVA rays, the primary culprits behind pigmentation and skin ageing, cut straight through clouds and glass. That means your skin is exposed on overcast UK days, on your daily commute, and even when you’re just sitting by a window at home or in the office.
To get it right, here’s what you need to do:
- Choose Broad-Spectrum: Your sunscreen absolutely must protect against both UVA and UVB rays. UVB is what causes sunburn, but it’s the deeper-penetrating UVA that really kicks off the pigment-producing process that leads to sun spots.
- Aim for at least SPF 30: For everyday protection, SPF 30 is the recommended minimum. However, if you’re serious about preventing pigmentation, SPF 50 gives you that extra bit of security.
- Apply Enough, and Apply Again: Here’s where most people go wrong—they don’t use enough. You need about half a teaspoon just for your face and neck to get the protection stated on the bottle. Reapplication is also key; top up every two hours if you’re outdoors, and more often if you’ve been swimming or sweating.
Consistency is everything, and the only way to be consistent is to find a formula you genuinely enjoy using. To help you navigate the options, you can learn more about selecting the perfect sunscreen that fits your skin and lifestyle.
Think of sunscreen as the final, non-negotiable step in your morning skincare routine. Applying it every single day, without fail, is the most effective investment you can make in maintaining an even skin tone.
Adopt a Gentle Skincare Routine
Beyond the sun, the other key to prevention is keeping inflammation to a minimum. Remember post-inflammatory hyperpigmentation (PIH)? That’s the lasting mark left behind after irritation. Aggressive scrubbing, harsh products, and—we’ve all been tempted—picking at spots are all major triggers.
A gentle, nurturing approach is always best. Avoid the temptation to over-exfoliate or pile on products with high concentrations of irritating ingredients. The best thing you can do is listen to your skin. If it feels tight, looks red, or stings, that’s a clear signal to pull back. By keeping your skin calm and happy, you dramatically reduce the risk of inflammation leaving its mark behind.
Proven Treatments for Fading Dark Spots

Once those dark spots have made an appearance, the best way forward is a consistent, well-thought-out treatment plan. We’re essentially fighting a battle on two fronts: first, to fade the discolouration you can already see, and second, to put a stop to the pigment production that’s creating new spots.
This means calling in specific active ingredients that intervene at different stages of the pigmentation pathway. Some work by blocking melanin production at the source, while others focus on speeding up the shedding of already-discoloured skin cells. It’s all about a combined, strategic approach.
Key At-Home Skincare Ingredients
The absolute cornerstone of tackling hyperpigmentation at home is building a routine packed with the right active ingredients. And let me be clear: consistency will always win out over intensity.
Here are some of the most effective, evidence-backed ingredients you should have on your radar:
- Retinoids (Vitamin A): Often called the gold standard in dermatology, and for good reason. Retinoids act like a traffic controller for your skin cells, speeding up their turnover. This process pushes pigmented cells to the surface faster so they can be sloughed away, revealing brighter skin underneath.
- Vitamin C (L-Ascorbic Acid): Think of this as your skin’s personal bodyguard. As a powerful antioxidant, Vitamin C protects against the free radical damage that can trigger more pigmentation. But its real magic lies in its ability to inhibit tyrosinase – the key enzyme needed to produce melanin. It both fades existing marks and helps prevent new ones.
- Azelaic Acid: A true hero ingredient, especially for anyone dealing with the dark marks left behind by acne (post-inflammatory hyperpigmentation). It’s brilliant because it has anti-inflammatory properties and also acts as a tyrosinase inhibitor, gently fading discolouration without the irritation often associated with other acids.
- Niacinamide (Vitamin B3): This is a clever multi-tasker. Instead of stopping melanin production, niacinamide works by blocking the pigment’s journey from the melanocyte (the pigment factory) to your visible skin cells. The pigment is still made, but it has a much harder time showing up on your face.
A crucial piece of advice: go slow when introducing new actives. Start with one product at a time, using it just a few times a week. Only once your skin is happy should you build up to more frequent use. This is the best way to avoid irritation, which can ironically cause more inflammation and pigmentation.
Professional In-Clinic Procedures
For stubborn, deep, or widespread pigmentation, sometimes at-home skincare needs a professional boost. In-clinic treatments can deliver more dramatic and faster results, but they absolutely must be performed by a qualified dermatologist or aesthetic practitioner.
They will be able to properly assess your skin, diagnose the type of hyperpigmentation you have, and recommend the safest, most effective path forward. A proper consultation is non-negotiable. To get a better sense of what’s available, it’s worth exploring the range of professional dermatology treatments that tackle these concerns.
Chemical Peels
Don’t let the name intimidate you. Professional chemical peels use specially formulated acids (like glycolic, lactic, or mandelic) at higher, controlled concentrations to deeply exfoliate the skin. This effectively removes the top layers where the excess pigment is sitting, revealing the fresher, more evenly toned skin just below. If you’re curious about less intense versions, our guide breaks down the best at-home chemical peel options.
Laser Therapy
Lasers offer a high-tech solution, using focused beams of light energy that are specifically attracted to melanin. The energy shatters the pigment into tiny particles, which the body’s immune system then clears away, all without harming the surrounding skin. Different lasers work for different issues; for instance, Intense Pulsed Light (IPL) is great for superficial sun spots, while fractional lasers like Fraxel can target deeper pigment like melasma.
Microneedling
Also known as collagen induction therapy, microneedling is a fantastic procedure for improving overall skin health. It uses a device with ultra-fine needles to create thousands of tiny, controlled micro-injuries in the skin. This process kicks the skin’s natural wound-healing response into high gear, boosting cell turnover and collagen production, which helps to break up pigment and improve your skin’s texture and tone.
Common Questions About Facial Hyperpigmentation
Let’s wrap things up by tackling some of the questions I hear most often from clients dealing with dark spots. Getting some clear, practical answers can make all the difference in managing your expectations and feeling confident in your skincare plan.
How Long Does It Take to See Results?
This is the big one, and the honest answer is: it takes patience. When you’re consistently using great topical treatments like Vitamin C or a retinoid every day, you might start to see some initial brightening in about 4-8 weeks. But for that really noticeable fading, you’re looking at more like 3-6 months. Think of it like a marathon, not a sprint; your skin needs time to turn over new cells.
Now, in-clinic procedures like a chemical peel or laser treatment can definitely speed things up, and you might see a difference after just one session. But even then, a series of treatments is almost always needed to get the best possible outcome. And remember, deeper, more stubborn pigmentation like melasma will always take longer to shift than superficial sun spots.
Can Hyperpigmentation Disappear On Its Own?
Sometimes, but it’s a bit of a gamble. The lighter, more superficial marks left behind by a breakout—that post-inflammatory hyperpigmentation—can often fade on their own over several months to a year. The catch? That only happens if you are absolutely religious about wearing sunscreen every single day.
Unfortunately, sun spots from years of UV exposure and hormonal melasma very rarely go away without a proper treatment plan. Any time your skin sees the sun without protection, it’s going to darken those existing spots and put a stop to any natural fading. This is why a targeted routine and strict sun care are non-negotiable.
The single biggest mistake people make is underestimating the sun. One afternoon without sunscreen can undo weeks of hard work, especially if you’re prone to melasma or post-inflammatory marks.
Are Natural Remedies Like Lemon Juice Safe?
It’s so tempting to reach for a quick DIY fix from the kitchen, but please, steer clear of things like neat lemon juice. At best, it’s ineffective; at worst, it’s downright harmful. The high acidity can give you a chemical burn, and it can also trigger something called phytophotodermatitis—a nasty skin reaction that, ironically, makes hyperpigmentation much worse when the skin is exposed to sunlight.
If you have sensitive skin, these harsh DIY methods can cause a lot of inflammation, which is the last thing you need. A much safer and more effective route is to explore gentle exfoliation for sensitive skin with products that have been professionally formulated to be both safe and effective. It’s always better to stick with proven, evidence-backed ingredients like azelaic acid or liquorice root extract.
When Should I See a Dermatologist?
I always recommend seeing a dermatologist if your dark spots are covering a large area, aren’t getting any better after a few months of using over-the-counter products, or are genuinely upsetting you. A professional can give you a proper diagnosis, rule out anything more serious, and offer prescription-strength treatments you can’t get otherwise.
Most importantly, if you ever notice a dark spot that changes in size, shape, or colour, or one that becomes itchy or starts to bleed, book an appointment immediately. These can be warning signs of skin cancer, and getting it checked by an expert is essential.
At Beauty Page, we provide a curated selection of professional-grade skincare solutions designed to address hyperpigmentation effectively and safely. From potent antioxidant serums to at-home chemical peels, find the perfect addition to your routine to achieve a clearer, more radiant complexion. Explore our advanced formulations at https://beautypage.co.uk.










